TYPES OF VACCINES AND HOW THEY ARE MADE?

What is a vaccine?
A vaccine is known as a biological medicine which provides active acquired immunity to a particular infectious disease. It typically contains an agent which
resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. It trains the body’s immune system to fight against a disease which has not come into contact with before. Generally, rather than treat a disease, vaccines are designed to prevent disease, once you have caught it by working with your body’s natural defenses to build protection. According to the WHO, there are vaccines to prevent more than 20 life-threatening diseases including diphtheria, tetanus, pertussis, influenza and measles.
They underpin global health security and will be a vital tool in the battle against antimicrobial resistance.
What is vaccination?
Vaccination is the process of administration of a vaccine to help the immune system to develop immunity from a particular disease. It is a safe, simple and effective method of protecting people against harmful diseases, before they come into contact with them. Interestingly, it uses the body’s natural defenses to build resistance against specific infections and eventually makes the immune system stronger. After vaccination, your immune system is trained to create antibodies, similarly it does when it is exposed to a disease. But since vaccines contain only killed or weakened forms of the microbe like viruses or bacteria, they do not cause the disease or put people at risk of its complications.
There are several routes of vaccine administration. They are,
- By mouth (Oral)
- By injection (intramuscular, intradermal, subcutaneous)
- By puncture
- By transdermal
- By intranasal
- By mouth (Oral)
Oral vaccination typically works by generating a large amount of secretory IgA (sIgA), which plays a major role in mucosal defense against pathogens that enter the body through mucosal surfaces and cause diseases of the respiratory, intestinal and genital tracts. Oral vaccines are safe, easy and efficient to administer. And also they are convenient for all ages. They have been successfully developed to protect from many oral transmitted infectious diseases. Some well known oral vaccines are the oral polio vaccine (OPV), rotavirus, cholera and some typhoid vaccines. Most of the currently available oral vaccines are based on heat-killed or attenuated pathogens. The disadvantage of these vaccines is that they do not provoke a sufficient immune response. As a result of that they do not result in pathogen persistence and disease progression in immunocompromised individuals.
- By injection (intravenous, intramuscular, intradermal, subcutaneous)
Most vaccines are given by using this method. Some of the advantages of vaccination by injections are their results have been proven, the protection is long-term and the availability of vaccines are high. The main drawback of these vaccines are their challenging administration process. The correct needle size should be chosen, when administering a vaccine by injection.
Intravenous (IV) injections. An IV injection is the fastest way to inject a medication and involves using a syringe to inject a medication directly into a vein. …
Intramuscular (IM) injections are administered into the muscle through the skin and subcutaneous tissue. This method allows the medication to be absorbed into the bloodstream quickly. Intramuscular injections are used when other types of delivery methods are not recommended. Hepatitis A and B, Hib are examples for intramuscular injections. When administering an intramuscular injection, a 90° angle is used and all of the vaccine is injected in the muscle tissue by 1 inch if possible.
Intradermal (ID) injections are administered into the dermis, just below the epidermis. Since they provide a local and very little systemic effect, they are commonly used for tuberculin skin testing. Other than that they can also be used for allergy testing and local anesthetics. When administering an intradermal injection, a 25- gauge or smaller needle is inserted just under the epidermis at an angle of approximately 10°.
Subcutaneous (SC) injections are administered into the fatty tissue found below the dermis and above muscle tissue. A SC injection is known as the best for giving certain medicines such as Insulin. IPV, MMR and VAR are examples for subcutaneous injections. When administering a subcutaneousinjection the needle should be inserted at a 45 to 90° angle to the pinched-up skin. And it is important that the needle is completely covered by skin.
- By puncture
There are 2 main methods called scratch method and multiple puncture method. The multiple puncture method has been recommended as the method of choice for smallpox vaccination and BCG vaccination for infants.
- By transdermal
Recently, transdermal techniques have been investigated for vaccines including COVID-19. This route offers an improved vaccine administration. Since it targets potent immune cell populations of the skin, it may lead to a strong immune response at much lower doses when compared with an injectable vaccine. The human skin is composed of two layers named epidermis and dermis and they are populated by dendritic cells (DCs), which are known as potent antigen-presenting cells (APCs). “Transcutaneous immunization has therefore become an attractive and alternative route for vaccination. Techniques such as sonophoresis, microneedle-assisted delivery, iontophoresis, and elastic liposomes are among those being used and developed for transdermal vaccine delivery.
- By intranasal
Intranasal vaccines are administered into each nostril using a manufacturer-filled nasal sprayer. Here, the patient asked to be seated in an upright position and instructed to breathe normally. In order to prevent inadvertent movement, the provider should gently place a hand behind the patient’s head. Proper hand hygiene (using gloves etc.) should be performed to administer the vaccine. Even Though the patient coughs, sneezes, or expels the dose in any other way, the dose does not need to be repeated. The influenza vaccines FluMist/Fluenz™ and the Nasovac™ live attenuated vaccine are two of the licensed intranasal vaccines for humans.
How are vaccines made?
There are different types of vaccines. But usually there is one thing in common among them. That is they are inherently biological. Vaccines are made up of whole bacteria or viruses, or parts of them, often a protein or sugar. These active components of the vaccine, called antigens, are what trigger an immune response when in the body. Vaccines are known as biological products. So, most of the conventional viral vaccines need to be grown on biological material. As an example,
- chicken eggs with influenza vaccines
- mammalian cells with hepatitis A vaccines
- yeast for hepatitis B vaccines
This process is somewhat laborious and slow. For example, when developing the flu vaccines, firstly, the live virus is injected into an embryonated egg. Then the virus replicates and the viral material is collected and followed by purification and inactivation. Newer RNA vaccine production by DNA template is much cheaper and faster than conventional vaccine production.
Vaccines are made with complex biological molecules which are inherently unstable and as a result of that, they are prone to degradation if left on their own. In order to avoid this, vaccines usually contain a few additives. This helps the vaccine to stay safe and effective from the manufacturing to their point of use. These additives contain several ingredients including preservatives, stabilizers, surfactants, diluents, residuals and adjuvants. Preservatives stop the vaccine from being contaminated once the vial has been opened while stabilizers stop any chemical reactions from happening. Sugar (e.g. lactose) or gelatin are two examples for stabilizers. Normally surfactants stop the components of the vaccine from clumping together. Diluents are liquid components which are used to dilute a vaccine to the correct concentration and sterile water is often used as diluent. Residuals are the components which are not deliberately added to vaccines. They are considered as leftover traces of the ingredients of the vaccine, and yeast or egg protein are some examples for residuals. Some of the vacancies contain adjuvants which boost the immune response to the vaccine. This is done either by ensuring the vaccine’s prolonged availability at the injection site or by stimulating local immune cells. When adjuvants are used, a lower dose of the vaccine needs to be used. Aluminium, which is below the threshold value of safety, is known as a common adjuvant in vaccines.
How do vaccines work?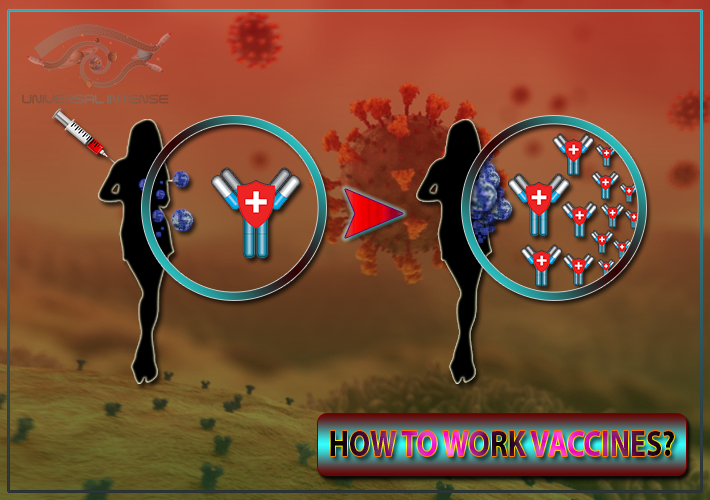 Vaccines generally work by stimulating a response from the immune system against a virus or bacterium. As a result of this a ‘memory’ is created in the immune system and this immune memory allows the body to ‘remember’ a specific pathogen such as virus or bacterium. So that the body can protect itself against this virus or bacterium and prevent disease that it causes. As mentioned before most vaccines contain a weakened or an inactivated (killed) form of a virus or bacterium that cannot cause disease. This is known as an antigen.
Vaccines generally work by stimulating a response from the immune system against a virus or bacterium. As a result of this a ‘memory’ is created in the immune system and this immune memory allows the body to ‘remember’ a specific pathogen such as virus or bacterium. So that the body can protect itself against this virus or bacterium and prevent disease that it causes. As mentioned before most vaccines contain a weakened or an inactivated (killed) form of a virus or bacterium that cannot cause disease. This is known as an antigen.
This antigen is recognized as foreign by the immune system when a person gets a vaccine. As a result of this, the immune cells are activated and they kill the disease-causing virus or bacterium and make antibodies against it. So, the immune cells – called T-cells and B-cells – in the blood, in the bone marrow and throughout the body are activated. This helps the immune system to remember if the person comes into contact with the actual virus or bacteria later. It can then produce the right antibodies and activate the right immune cells quickly, to kill the virus or bacterium. Eventually this protects the person from the disease.
Different vaccines bring about different levels of protection. How long protection lasts also depends on the disease it protects against. Some vaccines can only protect against a disease for a short period and may need booster doses; for others, immunity can last a lifetime.
Most importantly, vaccination does not only protect the ones who have received a vaccine. It also indirectly protects unvaccinated people in the community including children who are too young to be vaccinated or people with weakened immune systems through decreasing the risk of being exposed to infection. In order to generate this community immunity (herd immunity) it is important to vaccinate enough people in an area. In contrast, people who gain immunity by getting the actual disease can expose other people to the disease while putting themselves at risk of serious complications from the disease.
How effective is vaccination?
In order to measure the efficacy of a vaccine, a controlled clinical trial should be carried out. Then the ratio of developing the ‘outcome of interest’ (usually disease) among the vaccinated people is compared with that of among the people who got the placebo (dummy vaccine). In order to calculate the relative risk of getting sick the numbers of sick people in each group are compared once the study is complete. This depends on whether or not the subjects received the vaccine. Through this the efficacy can be taken as a measure of how much the vaccine lowered the risk of getting sick. A lot fewer people in the group who received the vaccine should become sick than the people who received the placebo if a vaccine has high efficacy.
Through the vaccine effectiveness someone can take a measurement of how well vaccines work in the real world. Even though clinical trials include a wide range of people including a broad age range, both sexes, different ethnicities and people with known medical conditions, still they cannot be considered as a perfect representation of the whole population. Since the efficacy observed in clinical trials applies to specific outcomes in a clinical trial, effectiveness in the real life conditions can differ from the efficacy measured in a trial. So, the efficacy of vaccination for a much bigger and more variable population can’t be predicted exactly.
Types of vaccines
- Live attenuated Vaccines (LAV)
- Inactivated Vaccines (Killed Antigen)
- Subunit Vaccines (Purified Antigen)
- Toxoid Vaccines (Inactivated Toxins)
- DNA / RNA Vaccines
Live attenuated Vaccines (LAV)
A weakened form of the disease-caused pathogen (bacteria or virus) is used in live- attenuated vaccines. This weakening is done by its genetic code alteration to prevent the rapid replication of the pathogen in human cells. Due to this weakening the pathogen no longer can cause the disease. But still the immune system is able to observe the morphology of the virus and create a long-lasting immune response. When considering COVID-19 vaccines, live- attenuated vaccines which contain the SARS-CoV2 virus have not been focussed by most scientists. Instead, they have tested previously generated live- attenuated viruses including the common cold and the measles virus which control the genetic code of the virus to display the key SARS-CoV2 spike protein. This is known as a subtype of live- attenuated vaccines called a viral-vector vaccine. Some of the examples for live- attenuated vaccines are MMR, Rotavirus, Chickenpox and Yellow fever vaccines.
Inactivated Vaccines (Killed Antigen)
Inactivated vaccines use a dead form of the disease caused germ which is killed by using heat and/or chemicals. Similar to the live- attenuated vaccine, the inactivated germ shows the immune system what the germ looks like without making the patient sick. Generally, the live- attenuated vaccine is stronger than an inactivated vaccine. So, an inactivated vaccine may require booster shots over time. Clinical trials of inactivated COVID-19 vaccines have tested for inactivated SARS-CoV2 virus. Hepatitis A, Flu, Polio and Rabies are some examples for Inactivated vaccines.
Subunit Vaccines (Purified Antigen)
The subunit vaccines contain only a key piece of the germ including protein or sugar which causes the disease and when the immune system contacts it, a strong immune response is developed. Generally, this piece is on the outer surface of the germ and for the effective use of these vaccines, it is important to identify the correct piece even though it is not trivial. When considering the COVID-19 subunit vaccines, scientists focused both on the spike, “S” protein which sticks out on the surface of the SARS-CoV2 virus and specific subunit vaccines which use virus-like particles (VLP) in order to display the subunit to the immune system. These particles contain a membrane, just as the actual SARS-CoV2 virus. Since these virus-like particles (VLP) have no genetic code within, they are not infectious. But the particles hold many subunits together which helps the immune system to identify the subunit. Some of the examples for subunit vaccines are Hepatitis B, HPV and Shingles.
Toxoid Vaccine (Inactivated Toxins)
Toxoid vaccines contain toxoids (as antigens) which induce an immune response against specific bacterial diseases including tetanus and diphtheria. Usually, they are known as extremely effective and safe vaccines against these bacterial infections since they give a long-lasting immunity which is induced by a course of toxoid vaccines. This causes an immune response against weakened versions of specific bacterial toxins which are known as toxoids. The body forms an immune response to the original toxin (maintained immunogenicity), by using toxoids. But the toxoid cannot lead to any toxicity or toxin-induced disease since the toxoid is a weakened form of the toxin. Especially, compared with other vaccines, toxoid vaccines have been identified as more stable and less susceptible to damage caused by temperature, humidity, or light.
DNA / RNA Vaccines
In a cell, protein production can be divided into two parts as transcription and translation. Firstly, DNA is transcribed into RNA and then translated into protein. A DNA or RNA vaccine is a type of a subunit vaccine, but the difference is instead of introducing a subunit (protein) into the body, this vaccine provides the specific genetic code (DNA or RNA) for the cells in order to produce the subunit itself. Since RNA or DNA can be produced more easily and inexpensively in a laboratory compared to a subunit, it is a great benefit. Other than that, RNA vaccines have the added advantage of no risk that the RNA will integrate into the patient’s own genetic code which could not happen with a DNA vaccine. When talking about the United States, currently they do not use any DNA or RNA vaccines because the technology is new. These vaccines have presented a relatively simple and exciting way to develop a COVID-19 vaccine.
What is a Covid-19 vaccine?
Types of Covid-19 vaccines
- Attenuated Vaccines
- Genetic Vaccines
- Protein Vaccines
- Viral-vector Vaccines
Attenuated vaccines for COVID-19
This type of vaccine contains the weakened SARS-CoV-2 virus. This is recognized by the immune system to trigger a response without causing COVID-19 illness. This response builds immune memory which enables the body to fight off SARS-CoV-2 in future. Attenuated vaccine is considered as a well-known approach for COVID-19 vaccines. But it requires time and extensive testing. The immune response generated by the attenuated vaccine resembles the natural infection.
Genetic vaccines for COVID-19
The vaccine contains a segment of genetic material of the SARS-CoV-2 virus which codes for a specific protein. This can be DNA or RNA. When the vaccine is administered, body cells use the genetic material from the vaccine to make the SARS-CoV-2 protein, which is recognised by the immune system to trigger a specific response. This response builds immune memory which enables the body to fight against the SARS-CoV-2 in future. The genetic material, RNA in Moderna and Pfizer/BioNTech vaccine, codes for a specific viral protein. The advantages of genetic vaccines are their low cost and fast development. But they may need to be stored at specific low temperatures. CureVac, Inovio Pharmaceuticals are still in clinical trials for genetic vaccines for COVID-19.
Inactivated vaccines for COVID-19
This type of vaccine contains the killed SARS-CoV-2 virus, which is recognised by the immune system in order to trigger a response without causing COVID-19 illness. As a result of this response, immune memory is built, so the body can fight off SARS-CoV-2 in future. In order to boost the immune response this vaccine may need to be administered with an adjuvant. Other than COVID-19, these inactivated vaccines are used in humans for influenza diseases. Sinovac, Sinopharm, Bharat Biotech are some of the approved inactivated vaccines for COVID-19. Shifa-Pharmed, Chinese Academy of Medical Sciences have also developed inactivated vaccines for COVID-19.
Viral vector vaccines for COVID-19
The University of Oxford/AstraZeneca vaccine uses this technology to protect against COVID-19. This type of vaccine uses an unrelated harmless virus which is modified to deliver SARS-CoV-2 genetic material. This delivery virus is known as the viral vector. After the administration, body cells produce a specific viral protein using the genetic material to produce a specific viral protein, which is recognised by the immune system and triggers a response. This response builds immune memory, which enables the body to fight off the virus in future. The advantage of viral vector vaccines is that they generate a strong immune response while they may need to be stored at specific low temperatures. Other than COVID-19, these viral vector vaccines are used in humans for Ebola virus. AstraZeneca/Oxford are some of the approved viral vector vaccines for COVID-19 in the United Kingdom and United States. Apart from that Jannsen, CanSino, Gamaleya viral vector vaccines have been approved for COVID-19 in other areas of the world.
Protein vaccines for COVID-19
This type of vaccine contains proteins from the SARS-CoV-2 virus, which are recognised by the immune system in order to trigger a response. As a result, this response builds immune memory, which helps the body to fight off SARS-CoV-2 in future. The proteins used in protein vaccines can be whole proteins, protein fragments, or many protein molecules packed into nanoparticles. This type of vaccine has good previous safety records and they are usually administered with an adjuvant to boost immune response. Other than COVID-19, these protein vaccines are used in humans against Hepatitis B virus. Novavax and Sanofi/GSK have developed protein vaccines for COVID-19.